By Dustin Berger, M.S.
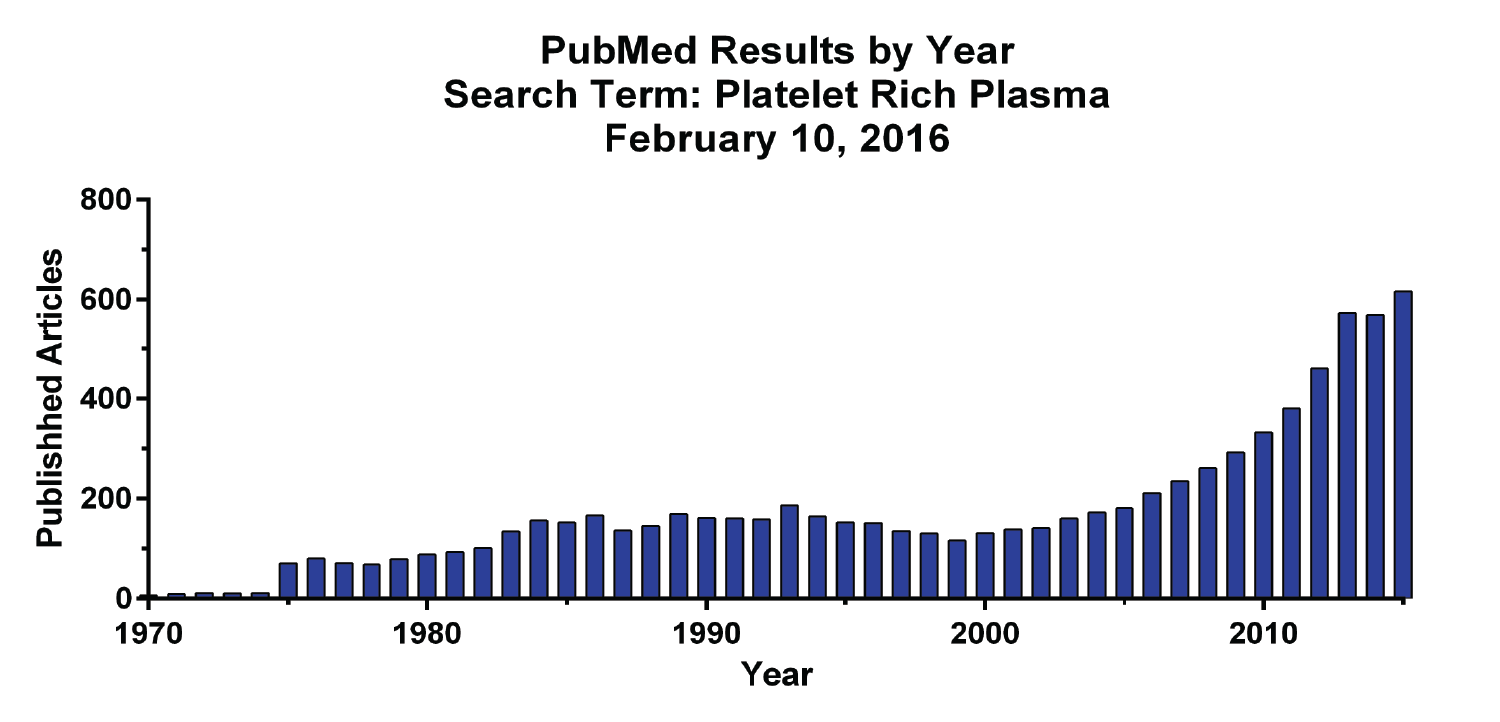
Platelets are small cell fragments within our blood that play important roles in the wound healing process. In addition to being responsible for stopping blood flow at a site of injury, platelets are loaded full of beneficial growth factors. Increased interest in platelet biology began over 40 years ago, with cell culture studies identifying platelets and their factors as the major serum components responsible for promoting cell growth1. By the late 1990s, several important growth factors were discovered within platelets, including platelet derived growth factor (PDGF), basic fibroblast growth factor (bFGF), transforming growth factor β (TGFβ), and vascular endothelial growth factor (VEGF)2. The increased knowledge of these easily accessible growth factors sparked the beginnings of a new therapeutic approach, a shift towards regenerative medicine. Platelet rich plasma (PRP), a plasma solution containing much greater levels of platelets than normally found in whole blood, was first used clinically in oral surgery patients to promote enhanced bone repair with positive results3. Thereafter, scientific interest in PRP has increased steadily, as evident by a recent PubMed search (below), and there are currently almost one-hundred open clinical trials involving PRP therapies to treat a variety of medical conditions, mostly of musculoskeletal origin (clinicaltrials.gov).
While PRP therapy has shown tremendous promise for promoting regenerative healing, not all PRP formulations are the same. Multiple factors play a role in the composition of the final PRP product, including the presence of other blood cell types (red and white blood cells), the method of platelet activation, and the final concentration of platelets isolated4. Nonetheless, recent laboratory reports have concluded highly concentrated platelet formulations to be detrimental to cultured connective tissue cells5,6. These results suggest that there may be a platelet concentration beyond which PRP therapies are no longer effective in stimulating tissue regeneration.
The Interventional Orthopedics Foundation (IOF) is committed to better understanding this phenomenon. Our research team is currently investigating how concentrated platelets and their associated growth factors affect the culture of human bone marrow derived stem cells (above) and the cells that form tendons. We are busy collecting data and will report back once a clearer picture on the effects of concentrating PRP emerges.
References:
1 Ross, R., Glomset, J., Kariya, B. & Harker, L. A platelet-dependent serum factor that stimulates the proliferation of arterial smooth muscle cells in vitro. Proc Natl Acad Sci USA 71, 1207–1210 (1974).
2 Textor, J. Platelet-Rich Plasma (PRP) as a Therapeutic Agent: Platelet Biology, Growth Factors and a Review of the Literature. Lecture Notes in Bioengineering (2013).
3 Marx, R. E. et al. Platelet-rich plasma. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 85, 638 (1998).
4 Amable, P. et al. Platelet-rich plasma preparation for regenerative medicine: optimization and quantification of cytokines and growth factors. Stem Cell Research & Therapy 4, 67 (2013).
5 Graziani, F. et al. The in vitro effect of different PRP concentrations on osteoblasts and fibroblasts. Clinical Oral Implants Research 17, 212 (2006).
6 Giusti, I. et al. Platelet Concentration in Platelet-Rich Plasma Affects Tenocyte Behavior In Vitro. BioMed Research International 2014, 1 (2014).